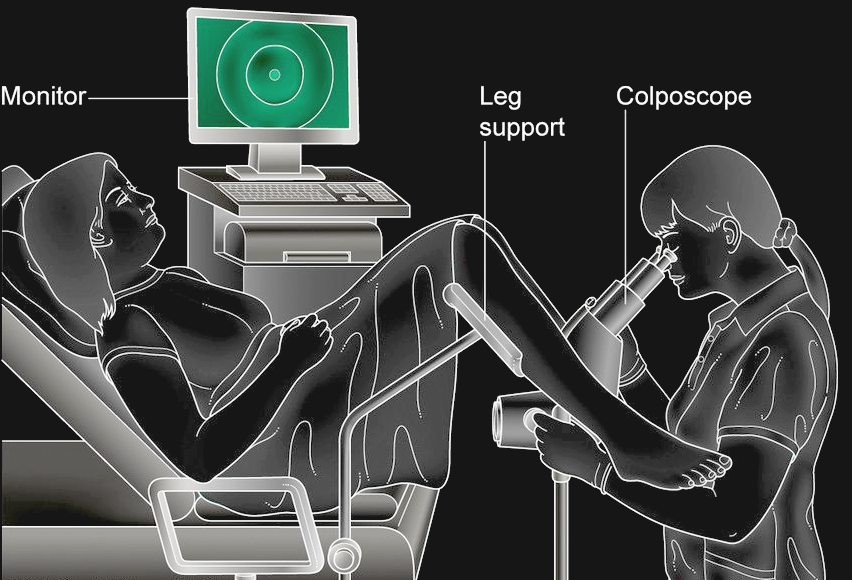
A colposcopy is carried out by a specialist called a
colposcopist. This may be a doctor or a specially trained nurse who may
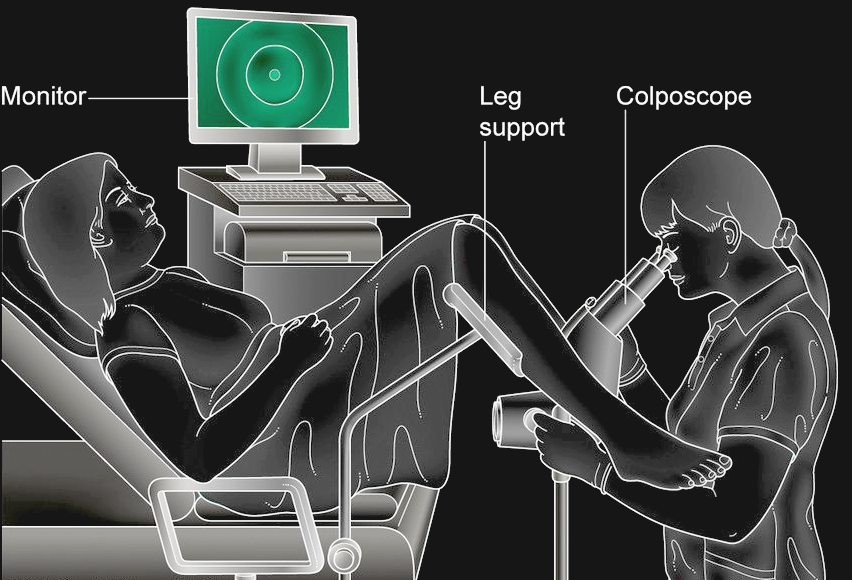
not be doing it right. During the procedure: you undress from the waist down (a loose skirt may not need to be removed) and lie down in a special type of chair with padded supports for your legs.
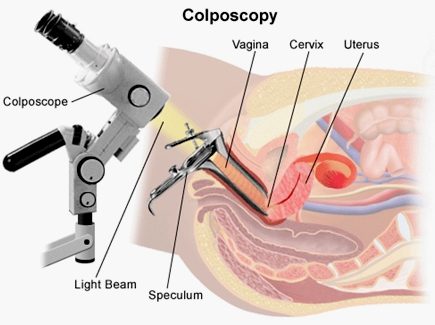
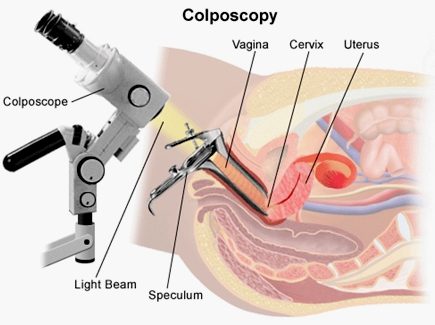
A device called a speculum is inserted into your vagina and gently opened similar to having a cervical screening test.
A microscope with a light (a colposcope) is used to look at your cervix this stays about 30cm (12 inches) outside your vagina and allows the colposcopist to see the cells on your cervix.
Special liquids are applied to your cervix to highlight any abnormal areas you may feel a mild tingling or burning sensation when these are applied.
A small sample of tissue (a biopsy) may be removed for closer examination in a laboratory this shouldn't be painful, but you may feel a slight pinch or stinging sensation.
If it's obvious that you have abnormal cells in your cervix, you may be offered treatment to remove the cells immediately. Otherwise, you'll need to wait until you get your biopsy
result.
After having a
colposcopy: you'll be able to go home as soon as you feel ready, usually straight afterwards.
You can return to your normal activities, including work and driving, immediately although some women prefer to rest until the next day.
You may have a brownish vaginal discharge, or light bleeding if you had a biopsy this is normal and should stop after three to five days.
Wait until any bleeding stops before having sex or using tampons, vaginal medications, lubricants or creams.
Your nurse or doctor may be able to tell you what they've found straight away.
If you have had a biopsy, it will be checked in a laboratory and you'll need to wait a few weeks to receive your result by post.
COLPOSCOPY
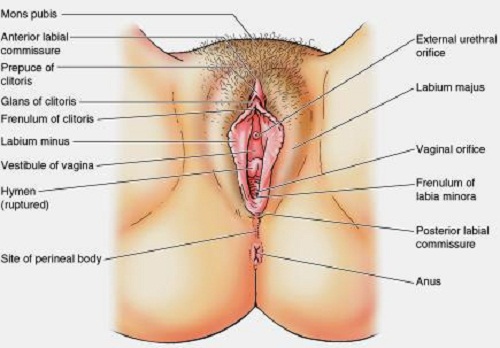
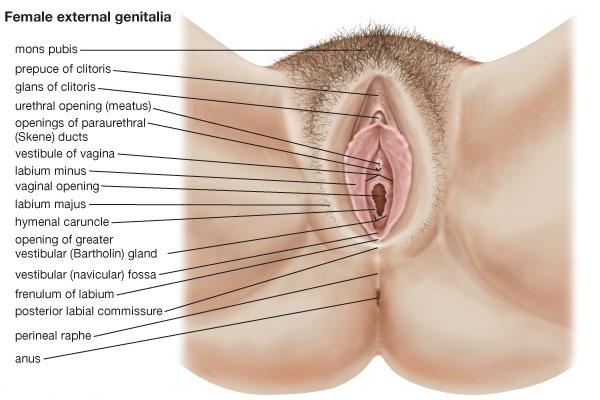
Colposcopy (Ancient Greek: κόλπος kolpos hollow, womb,
vagina + skopos "look at") is a medical diagnostic procedure to examine an illuminated, magnified view of the cervix and the tissues of the vagina and
vulva.
A specialized colposcope equipped with a camera is used in examining and collecting evidence for
victims
claiming to have been raped or sexually
assaulted. The technique should be
gainfully employed and developed to identify the growing numbers of false
allegations, so saving convictions based on testimony, that under the
present system, is all that is needed to send a man down. Dame
Butler Schloss is an advocate of enhancing our knowledge in this area
and said as much in her remarks on the above RCPCH guidance.
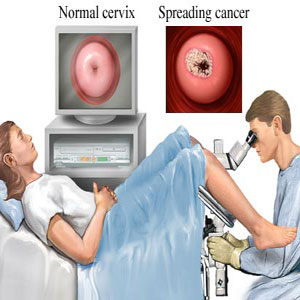
Many premalignant lesions and malignant lesions in these areas have discernible characteristics which can be detected through the examination. It is done using a colposcope, which provides an enlarged view of the areas, allowing the colposcopist to visually distinguish normal from abnormal appearing tissue and take directed biopsies for further pathological examination.
The
other use of colposcopy is to prevent cervical cancer by detecting precancerous lesions early and treating them. The procedure was developed in 1925 by the German physician Hans Hinselmann, with help from Helmut
Wirths.
PROCEDURE
During the initial evaluation, a medical history is obtained, including gravidity (number of prior pregnancies), parity (number of prior deliveries), last menstrual period, contraception use, prior abnormal pap smear results, allergies, significant past medical history, other medications, prior cervical procedures, and smoking history. In some cases, a pregnancy test may be performed before the procedure. The procedure is fully described to the patient, questions are asked and answered, and the patient then signs a consent form.
A colposcope is used to identify visible clues suggestive of abnormal tissue. It functions as a lighted binocular microscope to magnify the view of the cervix, vagina, and vulvar surface. Low power (2× to 6×) may be used to obtain a general impression of the surface architecture. Medium (8× to 15×) and high (15× to 25×) powers are utilized to evaluate the vagina and cervix. The higher powers are often necessary to identify certain vascular patterns that may indicate the presence of more advanced pre-cancerous or cancerous lesions. Various light filters are available to highlight different aspects of the surface of the cervix. Acetic acid solution and iodine solution (Lugol's or Schiller's) are applied to the surface to improve visualization of abnormal areas.
Colposcopy is performed with the woman lying back, legs in stirrups, and buttocks at the lower edge of the table (a position known as the dorsal lithotomy position). A speculum is placed in the
vagina after the vulva is examined for any suspicious lesions.
After a complete examination, the colposcopist determines the areas with the highest degree of visible abnormality and may obtain biopsies from these areas using a long biopsy instrument, such as a punch forceps, SpiraBrush CX or SoftBiopsy. Most doctors and patients consider anesthesia
unnecessary, save where multiple biopsy samples are to be taken - to decrease patient
discomfort.
The
results in sexual cases may have the same effect as a lie detector test,
save that the physical examination and photographic record are more
conclusive. If a girl has been raped, especially a young girl, there will
be signs that prove penetration (rape) has taken place. This will be especially
apparent in cases of non-consensual sex where no foreplay will mean no
lubrication and so increased trauma in the form of tearing (scars) and
bruising.
In
the case below, apart from the fact that the girl was "tightly
closed", there was also no signs of tearing of the fourchette, or
other trauma associated with digital penetration (without foreplay = dry).
The girl claimed regular assaults of this type that would have produced
scars and the like in 83% of cases, but there were no scars, a finding
which is clearly inconsistent with her claims.
A
partial notch was found in the hymen, but it is now known that such
findings are normal. Tears and the like in the hymen are full width if
caused by trauma, leaving scar tissue, rather than partial (a smooth small
indentation) as in naturally occurring
features. This was not explained to the jury, who were left believing that
there was no explanation for the 'notch' other than penetrative sex.
UNDERSTANDING
THE SEXUAL ABUSE EXAM - The "why"'s of the pediatric sex abuse
exam
It should assist physicians in evaluating what they see. It will also assist attorneys and members of the public who are required to evaluate reports.
Here is the proposed classification of anogenital findings in children as given by Adams (1994):
Normal (Class I)
* Periurethral bands
* Intravaginal ridges or columns
* Increased erythema in the sulcus
* Hymenal tags, mounds, or bumps
* Elongated hymenal orifice in an obese child
* Ample posterior hymenal rim (1-2 mm wide)
* Estrogen changes (thickened, redunant hymen)
* Diastasis ani / smooth area at 6 or 12 o'clock in perianal area
* Anal tag /thickened fold in midline
Nonspecific findings (Class II): May be caused by sexual abuse or other medical conditions.
* Erythema of vestibule or perianal tissues
* Increased vascularity of vestibule or hymen
* Labial adhesions
* Rolled hymenal edges in the knee-chest position
* Narrow hymenal rim, but at least 1 mm wide
* Vaginal discharge
* Venous congestion of perianal tissued, delayed in exam
* Fecal soiling
Suspicious for abuse (Class 3)
* Elarged hymenal opening - greater than 2 standard deviations from the nonabused study (McCann)
* Posterior hymenal rim less than 1 mm in all views
* Condyloa acuminata in a child
* Acute abrasions or lacerations in the vestibule or on the labia (not involving the hymen),
or perianal lacerations
Suggestive of Abuse / Penetration (Class 4)
* Combination of two or more suspicious anal findings or two or more suspicious genital findings
* Scar or fresh laceration of the posterior fourchette with scaring of the hymen
* Scar in peri-anal area, must take history into consideration* Clear Evidence of Penetrating Injury
* Areas with an absence of hymenal tissue, below the 3 o'clock to 9 o'clock line with patient supine,
which is confirmed in the knee-chest position
* Hymenal transections or lacerations
* perianal laceration extending beyond (deep to) the external anal sphincter
* Laceration of posterior fourchette, extending to involve hymen
* Scar of posterior fourchette associated with a loss of hymenal tissue between 5 and 7 o'clock.
The authors warn that this classification "does not represent a consensus of medical experts regarding the classification of findings with respect to abuse."
Here is a standard table for evaluating the overall likelihood of sexual abuse.
Notice that this table does not take into account the setting in which accusations are made, i.e., was there a previous custody battle?
In evaluating a report of sexual abuse, look for the following:
How was the exam performed? If the child is not relaxed, or labial traction and separation is not performed, the hymen may seem to be absent. Warm water may need to be applied to see the tissues clearly if they are stuck together. Blood and mucus may need to be wiped away. Was gonorrhea or chlamydia diagnosed? Only confirmed cultures are acceptable in court. Britton and ___ agree. Gram stain is nonspecific in the female at any age. Nonspecific bacterial infection of the vulva can look horrible, but it is quite common in young girls and does not indicate gonorrhea unless there are cultures to prove its cause. Was colposcopy performed? Are there photos? colposcopic examination and photographic documentation of the findings seems to be the standard of practice in the developed world. Adams and colleagues (1994) went through their files of 262 cases since July 1986 with convictions, and found only 18 without photos and 8 with only nonmagnified photos. Nowadays video is available as described by Finkel (1998).
It's normal to be normal. Fondling is not going to leave scars. Penetration of the hymen of a four-year-old girl by an adult man's penis will surely rupture the hymen. The literature is divided on the question of whether the latter can heal without a scar. If this is true, then the most horrible sexual abuse can give a normal exam, and physical findings can never exonerate a defendant. As a pathologist, I don't believe this. It doesn't make sense, and I have been unable to find a follow-up study showing that a Class V laceration has healed without a scar visible on colposcopy. This tells me something.
Some sex-abuse examiners never sign out an exam, "Physical findings do not match the story", although this is routine in forensic pathology of child abuse victims.
SANE
- SEXUAL ASSAULT NURSE EXAMINERS - USA
Recognizing the vital service that SANEs provide in sexual assault cases, some hospitals, like St. Mary's Hospital in Richmond, Virginia, have expanded their SANEs' role to include conducting evidentiary exams on domestic violence victims, accident victims, and other populations where forensic evidence may be
useful.
Use of the Medscope as an Alternative to the Colposcope
A colposcope magnifies genital tissue and is an important asset for the identification of genital trauma. Photographic equipment, both still and video, can be attached easily to the colposcope. In the legal arena, the use of the colposcope is well documented as an accepted practice in the examination of both child and adult sexual assault victims. The basic colposcope, without photographic equipment, costs between $10,000 and $15,000, although the price is falling as the technology becomes more available.
The medscope is an adapted dental camera and provides photographic documentation that has a greater depth of field than the colposcope and can be used to document injuries elsewhere on the
body. The complete medscope package is more affordable than the colposcope ($3,500 for the basic model and $11,500 including camera, internal lens, camera holder, monitor, printer, foot switch, VCR, and cart). Suzanne Brown, SANE Program Coordinator at Inova Fairfax Hospital, Virginia, noted that the medscope is portable and less cumbersome than the colposcope, is easier to operate, and takes digital prints instead of 35mm prints. Photographic images are taken using the foot instead of the hand, which frees the SANE's hands to conduct the exam and reduces the risk of contaminating the evidence. Digital images can be viewed on the monitor to make sure that they are well focused and clear whereas 35mm prints cannot be viewed prior to development. Digital prints, however, cannot be enlarged or reprinted like 35mm prints. The medscope does not have definite magnification ranges like the colposcope, but Brown indicated that the lack of this feature has not presented problems in court.
Uniform Statewide Colposcope and Forensic Equipment Protocols
New Jersey has recently implemented a statewide funding initiative to acquire identical, state-of-the-art forensic colposcope equipment for SANE programs participating in a Statewide Sexual Assault Standards Project. The project provides a specially designed forensic colposcope to all exam sites that are part of SANE programs approved and funded by the State Office of Victim/Witness Advocacy. The initiative is designed to maximize the ability to collect competent forensic evidence while supporting the provision of sensitive victim-centered care to sexual assault victims. The equipment consists of a traditional binocular colposcope with an advanced digital image-capturing system to enable the examiner to see the image quality before capture to ensure that high-quality, accurate photographic documentation is part of every forensic examination. Specially designed software has been developed to ensure the highest quality of photo documentation, evidence preservation, and the usefulness of the images for trial.
One of the important aspects of this program involves protocols providing for the strict confidentiality of evidentiary photographs taken, especially photographs of genital injury. The protocols provide that the images are secured with the program and not routinely printed and produced with a patient's forensic file. This helps to reassure victims who may be reluctant to proceed and allows the assurance of confidentiality to victims. Additionally, the security level of the specially developed forensic photo documentation software program eliminates the need to capture facial photographs when there is no injury to that area. The specially designed software provides the ability to securely transmit data and images for child and adolescent forensic sexual assault evaluations. Finally, the design and purchase of specialized equipment on a statewide basis allows for considerable price reduction and improves resource allocation by providing colposcopes to programs with limited funds.
Regional Programs
A regional SANE program is an important alternative to each locality having its own program from a staff training and competency perspective. By serving a larger regional area, SANEs will most likely see more clients, and each SANE will be able to complete a sufficient number of exams to develop and maintain clinical competence. Regional programs may be the only cost-effective way to provide SANE services in rural and remote areas where no one medical facility sees large numbers of sexual assault cases.
When the SANE program of Inova Fairfax Hospital in Virginia began in 1990, it took only adult cases in Fairfax County. It gradually expanded to serve child victims and widened its service area, allowing nurses to increase proficiency because they had more cases. It now serves a region of 20 jurisdictions. While some of these jurisdictions have SANE programs that handle adult cases locally, they tend to refer their cases of child sexual assault to the Fairfax
program.
The hospital-based SANE program in Bethel, Alaska, serves a remote region (three people per square mile) approximately the size of Oregon that is 400 miles from the state road system. Victims are transported by plane, boat, or snowmobile to the hospital. Between 130 and 150 exams are conducted each
year. The Matanuska-Susitna Valley SANE program is based at Valley Hospital in Palmer, Alaska, and serves a region the size of West Virginia. Since the region is on the road system, city police or Alaska State Troopers drive most clients to the SART center. The commute may take up to 3 hours. Since the SANEs from Palmer examine fewer than 50 cases per year, they are required to participate in case review meetings and to attend educational programs to maintain proficiency as forensic
examiners.
Child Sexual Abuse Diagnostic System
In rural or remote areas where SANEs may rarely see child victims, more experienced forensic examiners could assist SANEs in properly identifying and evaluating abnormalities. Better quality or more detailed evidence obtained through collaboration of numerous experienced clinicians could increase the likelihood of successful prosecution. The Fairfax, Virginia, SANE program is involved in a pilot project to develop a model regional diagnostic system for forensic examination of children who have been sexually abused. Using camera and computer-imaging equipment that is attached to the medscope, the nurse or physician conducting the forensic exam is able to immediately transmit photographic images of genital trauma to the computers of identified experts for their feedback during the examination. In addition to SANE programs, child advocacy center staff and pediatric emergency medicine specialists are participating in the
project. Although this model is still in the preliminary stages of development, it shows exciting promise. It has the potential to bring clinical expertise to every forensic evaluation of sexually abused children, regardless of the examination location.
Hymel and Jenny list the differential diagnosis of child sexual abuse.
Dermatology
Licneh sclerosus
Diapet dermatitis
Pinworms
Poor hygiene
Bubble bath
Nonabusive bruising
Seborrheic, atopic, or contact dermatitis
Lichen simplex chronicus
Lichen planus
Psoriasis
Bullous pemphigoid
Perianal venous congestion
Congenital
Labial fusion
Hemangioma
Midline defects
Prominent medial raphe
Linea vestibularis
Perianal hyperpigmentation
Midline anal skin tags
Diastasis ani
Injuries
Straddle injury
SPlitting injury
Female circumcision
Hair tourniquet
Seat belt or motor venicle accident injry to genitalia
Other
Behcet's disease
They also list the following as unlikely to be due to abuse:
Vestibular findings
Erythema
Lympnoid follicles on the fossa navicularis
Midline avascular areas of the fossa navicularis
Urethral findings
Periurethral bands
Urethral dilation with labial traction
Hymenal findings
Small hymenal mounds, projections or septal remnants with otherwise normal hymenal anatomy
Concavities of the hymen that are anterior, smooth, curved, and/or shallow
Imperforate hymen Labial findings
Small labial adhesions
More extensive labial adhesions in girls still in diapers
Midline avascular areas of the posterior fourchette
Intravaginal structures behind a normal hymen
Ridges
Rugae
CANDIA - THE MAJOR ARTICLES
Hymel KP and Jenny C., Child Sexual Abuse, Pediatrics in Review 17(7): 236-249, 1996. "A non-leading interviewe of the child often is the most critical component of the evaluation for suspected child sexual abuse." Also talks about standard-of-care. The words "consistent with" means "pretty good evidence, but not proof, of..."
Berent W., "Case Study: Allegations of Abuse Created in a Single Interview", J. Am. Acad. Child. Adol. Psych. 36(7): 966-70, 1998. A baby-sitter videotaped her grilling of a child. Ultimately the child reported that the father killed a pink cow and a pink horse with a gun. "An elaborate, detailed allegation was created through the use of repetitive, suggestive questioning." Dr. Berent is at 1601 Twenty-Third Avenue South, Nashville TN 37212.
Levitt, C., Further Technical Considerations Regarding Conducting and Documenting the Child Sexual Abuse Examination", Child. Abuse Neg. 22(6): 567-586, 1998. Carolyn Levitt MD is director of the Midwest Children's Resource Center, Children's Health Care, 360 Sherman Street Suite 200 St Paul MN 55102.
Bays J, Chadwick D, The medical diagnosis of the sexually abused child. Child Abuse & Neglect 17: 91-110, 1993.
Britton H & Hansen K, "Sexual Abuse", Clin Ob Gyn 40(1): 26-239, 1997. First author is at 100 N Medical Drive Suite 3400, Salt Lake City, Utah, 84133.
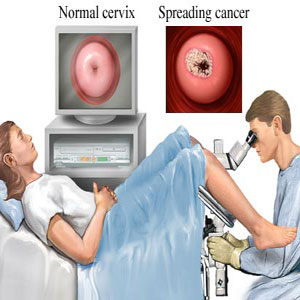
NHS
SCREENING
A
colposcopy is a simple procedure used to look at the cervix, the
lower part of the womb at the top of the vagina. It's
often done if cervical
screening * finds abnormal cells in your cervix.*
These
cells aren't harmful and often go away on their own, but
sometimes there's a risk they could eventually turn into cervical
cancer if not treated.
A
colposcopy can confirm whether cells in your cervix are abnormal and
determine whether you need treatment to remove them.
When a
colposcopy may be needed
You
may be referred for a colposcopy within a few weeks of cervical
screening if:
-
some
of the cells in your screening sample are abnormal
-
the
nurse or doctor who carried out the screening test thought your
cervix didn't look as healthy as it should
-
it
wasn't possible to give you a clear result after several screening
tests
A
colposcopy can also be used to find out the cause of problems
such as unusual vaginal bleeding (for example, bleeding after
sex).
Try
not to worry if you've been referred for a colposcopy. It's very unlikely
you have cancer and any abnormal cells won't get worse while you're
waiting for your appointment.
What happens
during a colposcopy
A
colposcopy is usually carried out in a hospital clinic. It takes about
15-20 minutes and you can go home the same day.
During
the procedure:
-
you
undress from the waist down (a loose skirt may not need to be removed)
and lie down in a special type of chair with padded supports for
your legs
-
a device
called a speculum is inserted into your vagina and gently opened
-
a microscope
with a light is used to look at your cervix this doesn't
touch or enter your body
-
special
liquids are applied to your cervix to highlight any abnormal
areas
-
a
small sample of tissue (a biopsy)
may be removed for closer examination in a laboratory this
may be a bit uncomfortable
If
it's obvious that you have abnormal cells in your cervix, you may
have treatment to remove the cells immediately. If this isn't clear,
you'll need to wait until you get your biopsy results.
Read
more about what
happens before, during and after a colposcopy.
Results of a
colposcopy
It's
often possible to tell you right away if there are any abnormal cells in
your cervix. But if you had a biopsy, it may take up to four to eight
weeks to get your results in the post.
The
result of your colposcopy and/or biopsy will be either:
-
normal
about 4 out of 10 women have no abnormal cells and are
advised to continue attending cervical screening as usual
-
abnormal about
6 out of 10 women have abnormal cells in their cervix and may need treatment
to remove them
Your
doctor or nurse may use the term CIN or CGIN when discussing your
biopsy result. This is this medical name for abnormal cells.
It's
followed by a number (for example, CIN 1) that indicates the chances of
the cells becoming cancerous. A higher number means a higher risk of
cancer developing if the cells aren't removed.
Read
more about colposcopy
results.
Treatments to
remove abnormal cells
Treatment
to remove abnormal cells is recommended if there's a moderate or high chance
of the cells becoming cancerous if left untreated.
There
are several simple and effective treatments that can be used to remove the
abnormal cells, including:
-
large
loop excision of the transformation zone (LLETZ) a
heated wire loop is used to remove the abnormal cells
-
a
cone biopsy a cone-shaped piece of tissue containing the
abnormal cells is cut out from your cervix
LLETZ
is usually carried out while you're awake but your cervix is numbed. You
can go home the same day.
A
cone biopsy is usually done under general
anaesthetic (where you're asleep) and you may need to stay in hospital
overnight.
Read
more about colposcopy
treatments.
Definitive for Sexual Abuse
* Presence of sperm (I would have added "Presence of prostate-specific antigen and/or
prostatic acid
phosphatase" - Ed.)
* Gonorrhea or syphilis not transmitted congenitally
* HIV not transmitted neonatal or intravenously
* Pregnancy, not consensual with a peer
* Acute unexplained aotenital injury or isolated hymenal trauma
* Definite unexplained hymenal transections, healed or acute, "absent hymen"
I would have added bite marks, petechiae, avulsions, hematomas, or contusions in the vulva or the anus,
without some good explanation.
- Ed.
Other experts list "absent hymen" as merely "consistent with".
Highly Suggestive
* Chlamydia, conduyloma acuminatum, trichomonas not neonatally acquired
* Anogenital herpes herpes, not neonatally transmitted or accompanying stomatitis
* Posterior/lateral angular clefts or tears of hymen
* Nonmidline anal scars or tags
* Dilation of anal opening to >15 mm within 30 sec with no stool present
Suspicious for Sexual Abuse
*
Nonspecific vaginitis (bacterial vaginosis)
* Posterior narrowing (<1 mm) or asymmetry of hymen
* Healed unexplained injry to fossa or posterior fourchette
* Decreased thickened anal folds
* Thick irregular labial adhesions not related to hygiene or diapering
Finkel, MA, "Technical Conduct of the Child Sexual Abuse Medical Examination", Child Abuse & Neglect 22(6): 555-566, 1998. Historical aspects, including a description of how the early examiner's opinions "were frequently quoted and accepted as scientific fact." Much on the value of colposcopy. Deplores the fad for using the transverse diameter of the hymenal orifice as the gold standard for abuse. Finkel lists as unanswered questions, "What is the minimal acceptable use of technology to conduct and document an examination of an alleged child sexual abuse victim?" "Are observers more conservative in their interpretation of physical findings if there is an opportunity for a second opinion review of their observations and the potential for challenge?" and "What is the clinical relevance of the transverse hymenal orifice diameter?" It ends with a note on barriers to research, including the fact that there is not a full consensus on what is abnormal.
AACAP Official Action, "Practice Parameters for the Forensic Evaluation of Children and Adolescents Who May Have Been Physically or Sexually Abused", J. Am. Acad. Child Adolesc. Psych., 36(3): 423-438, March 1997. At last, the psychiatrists set standards for history-taking and evaluating the accuracy of statements from children. Agrees that most allegations are true, but lists causes of error.
Adams, JA et al., "Examination Findings in Legally Confirmed Child Sexual Abuse: It's Normal to be Normal", Pediatrics 94(3): 310-317, 1994. Contact Joyce A Adams, Dept of Pediatrics, Valley Medical Center 445 S Cedar Ave, Fresno CA 93702. Surprisingly, the group discovered that no correlation between genital findings and the child's report of having been penetrated. What disturbs me most about this article is the assumption that if somebody was convicted, abuse actually occurred. The authors state, "We must rely upon the child's description of the molestation as the best method of characterizing the abuse." So much for the semi-science of pathology. And ironically, there is no attempt to match the child's description with the findings. For some reason they didn't examine all their cases either.
Ed Friedlander MD
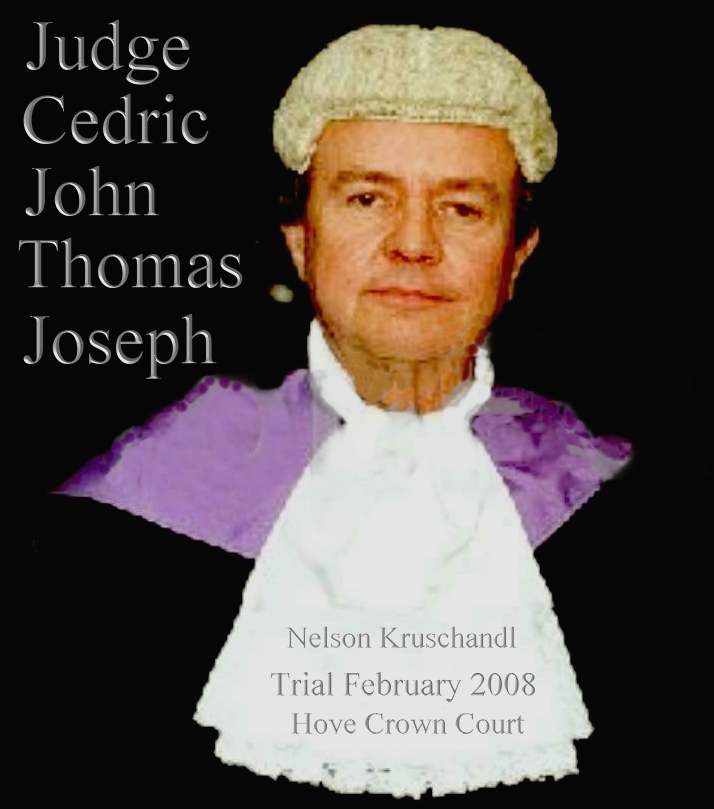
TEN
YEARS AND COUNTING - Oh
dear me. Dr Liebenberg was an expert witness in the case below alleging rape. Sometimes
experts think that are doing the right thing by not following the correct
procedures and not telling it like it is with new guidance about to be
published. The girl in this claim was examined in 2006 using old thinking to compile a
report. The trial below was held in February of 2008. In March of 2008
the above guidance was issued. In this guidance, the correct procedure for
examining claimants is spelled out. We wonder if dear old Melanie had seen
this document in draft form before giving her evidence. If so, that would
compound the misdirection that the jury were given and that would be fraud.
If not, then it is a curious coincidence that Liebenberg failed to conduct
her examination in a manner that would benefit the defence, but would most
assuredly disadvantage the defendant. As reporters, we have seen the good
doctor's report from 2006. In this report Liebenberg says that Claimant H
was: "Tightly closed and could not be opened with labial
traction." Here she was referring to the girl's hymen. We have also
read the above Guidance, and in those pages it is clear that if a girl is
interfered with more than once, her hymen will not be tightly closed.
There is a reliable method of measuring virginity, using the distance from
the hymen to the vaginal wall. The instrument used is called a Colposcope.
In this case the examiner did not obtain the adolescent's medical history,
so did not know that she had a congenital birth defect, which fortunately
she could not have attributed to the defendant.
It is important
when constructing a jigsaw puzzle, to have all the pieces. For example,
the examiner did not know that there had been heated exchanges between the
defendant and her mother and that he'd recently called off an engagement.
The girl was also a gymnast and previously rode horses. None of the Class
3-4 signs were present, as one might have expected if as claimed, the girl
had been regularly penetrated. The trial judge told the jury this might
have been on 40 occasions - thus virtually instructing the jury to
convict.
Dr
Liebenberg failed to mention to the jury that none of the expected
lacerations, transections and/or healed scars to the fossa or posterior
fourchette - or angular clefts or tears, or labial adhesions of the hymen
were present. She might have mentioned that the absence of any and all of
these signs, given the claimed regularity of abuse, was not consistent
with the allegations. But stands to be considered as part of a conspiracy
to pervert the course of justice. Dr Liebenberg could have mentioned that had any of
these signs been in evidence, that would have been either definitive proof
of sexual abuse or at best highly suspicious circumstances. But, as we
stress - none
of these were present and the jury had a right to know that before
sending a man to prison.
This
evidence does not stand alone. There is a diary that casts doubt as to
opportunity which the girl's mother hid in her loft so that the police
would not find it. On the stand under duress the girl's mother revealed
its existence, but then she knew that the defence would not have time to cross reference the
dates in it with the girl's testimony. Judge Cedric Joseph then wrongly told the
jury that this diary was the defendants - and still the CCRC
turn a blind eye.
Compounding
that crafting of the evidence, Gordon
Staker, James Hookway and Jo
Pinyoun failed to either secure or mention the existence of the
defendant's diaries, wherein the claimant's mother, a community
psychiatric nurse had written in her own hand that the accused should not
forget Valentines
Day.
The
plot thickens where solicitor Timothy
Stirmey and barrister Julian
Dale were provided with the diary entries, the accused pointing out
that the entries were written in his diaries by the mother of the
claimant, but his legal team failed to use this evidence in rebuttal of
the claim that a Valentines
Day Card sent to the claimant was in respect of the insistence of the
claimant's mother to cheer her daughter up. This was because the claimant
did not have a boyfriend and was not popular at school with the opposite sex.
What
possible excuse could Stirmey and Dale give for not putting this vital
information before the Jury? We can only think of one thing, that a deal
had been done with Sussex police
and the CPS,
not to include any evidence that would upset the chances of the Crown
obtaining a conviction. We know that Julian Dale was Eastbourne based and
we know that the father of the jilted
mother was a mason with the Tyrian
Lodge in South Street, 100 yards away from Eastbourne police station
at the top end of Grove Road.
We
imagine that once these facts are known by Melanie Liebenberg, that she
will have a tough time wrestling with her conscience, knowing that she
helped Sussex police to craft the
evidence in such blatant fashion. We hope then that she is not on the
payroll and might have the decency as a human
being to come forward and tell her story.
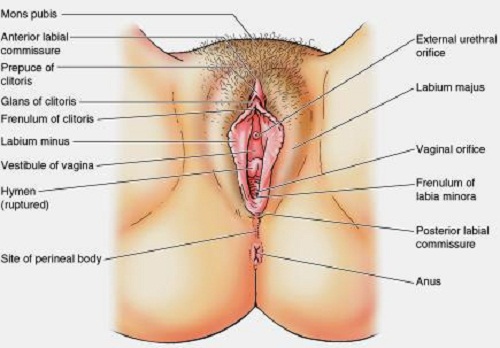
VIRGINITY
TESTING
A virginity test is the practice and process of determining whether a female person is a
virgin, i.e., whether she has never engaged in sexual intercourse. The test involves an inspection of a female's hymen, on the assumption that her
hymen can only be torn as a result of sexual intercourse.
TWO FINGER TEST
The process of virginity testing varies by region. In areas where medical doctors are readily available, such as Turkey before the country banned the practice, the tests will often be given in a doctor's office. However, in countries where doctors are not available, testers will often be older women, or whoever can be trusted to search for a hymen. This is common among African tribes that perform the test.
Another form of virginity tests involves testing for laxity of vaginal muscles with fingers (the "two-finger test"). A doctor performs the test by inserting a finger into the female's vagina to check the level of vaginal laxity, which is used to determine if she is "habituated to sexual intercourse". However, the usefulness of these criteria has been questioned by medical authorities and opponents of virginity testing because vaginal laxity and the absence of a hymen can both be caused by other factors, and the "two-finger test" is based on subjective observation. In virginity tests, the presence of a hymen is often used to determine if a woman is a virgin.
MARRIAGE
Some cultures require proof of a bride's virginity prior to her marriage. This has traditionally been tested by the presence of an intact hymen, which was verified by either a physical examination (usually by a physician, who would provide a certificate of virginity) or by a "proof of blood", which refers to vaginal bleeding that results from the tearing of the hymen. The physical examination would normally be undertaken before the marriage ceremony, while the "proof by blood" involves an inspection for signs of bleeding as part of the consummation of
marriage, after the ceremony.
RELIABILITY
Virginity testing is not a reliable indicator of a female having actually engaged in sexual intercourse because the tearing of the hymen may have been the result of an involuntary sex act, such as rape, or other event. Many researchers note that the presence of an intact hymen is not a reliable indicator of whether a female has been vaginally penetrated.
The hymen is a corona of thick skin situated just outside the vaginal canal, surrounding the entrance but in no way covering the
vagina, and is better described as a "vaginal corona" rather than "membrane" or "film". It is highly flexible and can be stretched or torn during every engagement in vaginal intercourse. It is a misconception that the hymen always tears during first intercourse. If the woman is not aroused, the hymen will not be as elastic as if it is moist due to arousal, and the risk increases for the corona to be damaged, which often is the case during the first intercourse.
IMMIGRATION
The United Kingdom had a policy to use virginity testing on women who said they were immigrating to marry their fiancees who were already living in the country. The
British government believed that if the women were virgins, they were more likely to be telling the truth about their reason for immigrating to the country. The policy ended in 1979.
VIRGINITY
TESTING - The
Zulu tribes in South Africa invite girls to prove that they are virgins, reviving an African tradition seen by many as the answer to the scourge of AIDS.
Bare-breasted teenagers wearing nothing but strings of beads and loincloths regularly submit to the ordeal of having a stranger check if their hymens are
intact - then leaping for joy when the test confirms that they are still
intact. Advocates say the revival of the rite is the most effective way to stop the spread of teenage pregnancies and the deadly HIV virus, believed to affect one in 10 South Africans.
It's no different to young girls of 13 in the UK asking their doctor for
the contraceptive pill, except that we give it to them. Who is doing
things correctly here! Girls who pass get white stars pasted on their foreheads and a certificate confirming their virginity.
Physical virginity tests were also reported in India from August 2009.
LINKS
& REFERENCE
https://web.archive.org/web/20100111122628/http://www.ojp.usdoj.gov/ovc/publications/bulletins/sane_4_2001/welcome.html
https://en.wikipedia.org/wiki/Colposcopy
https://www.nhs.uk/conditions/Colposcopy/
http://womenshealth.about.com/cs/cevicalconditions/a/colposcopy.htm
http://en.wikipedia.org/wiki/Virginity_test
http://en.wikipedia.org/wiki/Virginity_fraud
Colposcopy
Medical
conditions colposcopy
Virginity
tests zulu south africa
THE
ULTIMATE RAPE - ANATOMY
OF A STITCH UP - FLOW CHART - REAL LIFE INJUSTICE
|
|
ALLEGATION
SEXUAL ASSAULT 2006
follows
acrimonious family break up
|
|
|
|
|
|
|
|
|
|
TEACHER
loses
her note of original version of events
|
FRIENDS
report
their version of gossip
|
SOCIAL
WORKERS
failure
to investigate claims
|
|
|
|
|
|
|
|
|
|
CHILD
PROTECTION UNIT (Breaches SOCAP procedures)
|
|
|
|
|
|
|
|
|
|
2nd
OFFICER
|
|
INVESTIGATING
OFFICER
failure
to secure crime scene evidence
|
|
3rd
OFFICER
|
|
|
|
|
|
|
|
|
|
PATIENTS
DOCTOR
|
MEDICAL
EXAMINATION
uses
out of date forensic guidance in a controversial area of science
- defence barrister fails to challenge
|
PSYCHOLOGIST
|
|
|
|
|
|
|
|
|
|
|
|
DEFENDANT
CHARGED
Eastbourne
Magistrates Court
|
|
|
|
|
|
|
|
|
|
|
|
|
CPS
WITNESSES
Barrister
fails to apply to question claimant
|
|
|
|
|
|
|
|
|
|
|
|
FRIENDS
|
DEFENCE
WITNESSES
Barrister
fails to interview any of 17 witnesses for defence
|
FAMILY
|
|
|
|
|
|
|
|
|
|
|
|
MEDICAL
EVIDENCE
Barrister
fails to challenge medical evidence even after Lewes Crown Court
Judge tells him to get on to it.
|
|
|
|
|
|
| |
|
|
|
|
|
SX
POLICE
Refuse
to return defence computer evidence or to confirm nothing
untoward on computers. Court eventually force Police to return.
|
|
|
|
|
|
|
|
|
|
|
|
|
TRIAL
COURT FEB 2008
Hove
Crown Court - conservative venue with high conviction rate
|
|
|
|
|
|
| |
|
|
|
SOLICITOR
Cramp
& Co
|
BARRISTER
Sussex
Chambers
|
JURY
SWORN IN
|
BARRISTER
|
SOLICITOR
|
|
|
|
|
|
|
|
|
ARGUS
|
BECKETT
GROUP
|
PRESS
Publish
mid-trail in violation of Court Order to preserve fair hearing -
contempt of Court. Trial Judge, Cedric Joseph, fails to remedy.
|
SX
EXPRESS
|
KENT
& SX COURIER
|
|
|
|
|
|
|
|
|
|
|
JUDGES
SUMMING UP
|
|
|
|
|
Misdirects
Jury on vital diary evidence and asks them to decide medical
issues for which no juror is qualified
|
|
|
|
|
|
|
|
|
|
|
|
VERDICT
FEB 6 2008
A
guilty verdict is returned
|
|
|
|
|
JUSTICE
|
|
|
INJUSTICE
|
|
|
|
APPEAL
PROCESS BEGUN MAY 2008
|
|
|
APPEAL
SOLICITOR
Stuart
Grace Associates |
| |
1st
APPEAL BARRISTER
Michael
Harrison |
|
|
|
APPLICATION
TO COURT OF APPEAL requesting transcript of medical testimony |
|
|
|
|
|
| |
|
|
|
|
Her
Majestys's Court Service (HMCS) - refused transcript = abuse of
process Appeal barrister unable to perfect grounds |
|
|
|
|
| |
|
|
|
|
|
SINGLE
JUDGE
Sir
Christopher Holland - refuses leave and initials box -
compounding abuse of process
|
|
|
|
|
|
|
|
|
|
|
|
|
APPLICATION
TO ECHR May 2009
28536/09
|
|
|
|
|
|
|
|
|
|
|
|
APPLICATION
TO CCRC December 2009
In
England once leave to appeal is refused, there is no other
appeal process save via the Criminal Cases Review Commission
|
|
|
|
|
|
|
|
|
|
|
|
LEGAL
AID APP FUNDING 2010
|
|
|
|
|
|
| |
|
|
|
SOLICITOR
(CCRC)
Wells
Burcombe & Co |
| |
BARRISTER
(CCRC)
Dominic
Chandler |
|
|
|
CCRC
2010
Provisionally
refuse application. |
|
|
|
|
|
| |
|
|
|
|
|
CCRC
2010
Freedom
of Information request reveals new medical guidance exists which
the CCRC had neglected to mention |
|
|
|
|
|
|
|
|
|
|
|
|
LEGAL
AID APP FUNDING 2011
For
report as to natural marks and virginity reference RCPCH
guidance March 2008 - one month after trial.
|
|
|
|
|
|
| |
|
|
|
SOLICITOR
Ross
Simon & Co
Chizzy
Nsofor |
| |
BARRISTER
Lucy
Corrin |
|
|
|
|
|
|
|
|
|
|
CCRC
2011
Obtain
limited forensic Report as to naturally occurring marks.
|
|
|
|
|
|
| |
|
|
|
|
|
CCRC
2012
Admit
medical evidence to Jury misleading - but refuse to investigate virginity
issue, diary misdirection or provide transcript they have
obtained as to revelation of diary mid-trial. |
|
|
|
|
|
|
|
|
|
|
|
|
LEGAL
AID APP FUNDING 2012
To
seek a Judicial Review of CCRC's refusal to investigate
inconsistencies in evidence as above.
|
|
|
|
|
|
| |
|
|
|
SOLICITORS
JUDICIAL REVIEW
David
Wells & Siobhan Tipper |
| |
BARRISTER
Stephen
Field |
|
|
|
| |
|
|
|
|
|
HIGH
COURT (ADMIN) 2013
Refuse
leave for a Judicial Review
|
|
|
|
|
|
| |
|
|
|
|
|
LEGAL
AID REFUSE FUNDING
To
Appeal to the Appeal or Supreme Court
|
|
|
|
|
|
| |
|
|
|
CCRC
ECHR 2014
Fresh
Applications having exhausted possible domestic remedies |
|
|
|
|
|
| |
|
|
|
|
|
THREATS
OF RECALL 2015
License
conditions were used to prevent fresh application to the CCRC
until after the licence term had been served. |
|
|
|
|
|
| |
|
|
|
|
|
CCRC
2016
Fresh
application to the CCRC imminent. Virginity and Fraud will be
the next subjects for investigation. |
|
|
|
|
|
| |
|
|
In
a case where sexual assault is claimed, it is vital for investigators to
act quickly to prevent potential witnesses from rehearsing and developing
a version of a false claim. The investigators in this case allowed the
claimant two weeks to rehearse a story, all the while she was obtaining
feedback from social services and friends as to what to say such that it
might be acceptable (believed). Coaching or rehearsing a story is of
course illegal. Clearly, in this case coaching is a major feature. SOCAP
procedures are designed to prevent coaching by obtaining a statement the
moment an allegation is made. By this means false allegations may be
revealed by preventing changes to a story that repair obvious lies that a
defence will be able to disprove. We are following this Sussex case and
will report news as it happens.
LINKS
& REFERENCE
https://www.jostrust.org.uk/information-colposcopists
https://www.sccps.org/colposcopists/
https://www.documentcloud.org/documents/2081513-microscopy-of-hair.html
https://www.ncjrs.gov/pdffiles1/nij/grants/228091.pdf
http://twitter.com/edpilkington
http://www.telegraph.co.uk/Romford-and-Eastbourne-hospitals-dragged-in-to-NHS-care-scandal.html
http://www.lushingtonclinic.co.uk/consultants/dr-melanie-liebenberg/
www.drfosterhealth.co.uk/consultant-guide/Dr-Melanie-Anne-Liebenberg

Jos Cervical Cancer
Trust
CAN
Mezzanine
7-14 Great Dover
Street
London, SE1 4YR
Tel: 020 3096 8100
Email: info@jostrust.org.uk
Fundraising and donations: fundraising@jostrust.org.uk
Press and media: media@jostrust.org.uk
This
site is protected under Article10
of the European Convention on Human
Rights and Fundamental Freedoms.
FAIR
USE NOTICE
This
site contains copyrighted material the use of which has not always been
specifically authorized by the copyright owner. We are making such
material available in our efforts to advance understanding of
environmental, political, human rights, economic, scientific, and social
justice issues, etc. We believe this constitutes a 'fair use' of any such
copyrighted material as provided for in section 107 of the US Copyright
Law. In accordance with Title 17 U.S.C. Section 107, the material on this
site is distributed without profit to those who have expressed a prior
interest in receiving the included information for research and
educational purposes.